Watching someone you care about grapple with anxiety can feel incredibly helpless. You see the loop of worry, the physical symptoms, and the way it shrinks their world. Your first instinct is probably to jump in and try to fix it.
But what if the most powerful thing you can do isn't to provide answers, but to offer your presence?
This guide is built on a foundation of hope—the firm belief that with the right support, anyone can learn to manage their anxiety and live a full, meaningful, and panic-free life. Your role in this journey is more important than you know. You can be the anchor in their storm, the calm voice that reminds them that healing is possible and the waves will eventually settle. It all starts with understanding that anxiety is more than just feeling nervous; it's a complex and often exhausting condition, but a treatable one.
The Power of Validation and Patience
One of the most meaningful ways to help is to simply validate their feelings. When you say things like, "That sounds incredibly difficult," or "I can see how much this is affecting you," you’re communicating that you believe their experience is real and valid. This simple act of acceptance can defuse the secondary anxiety many people feel—the fear of being judged for what they're going through.
Patience is the other side of that coin. Healing isn't a straight line. There will be good days and bad days, steps forward and steps back. Try to avoid showing frustration or disappointment if they have a setback.
The goal isn't to erase their anxiety overnight, but to stand with them as they learn to navigate it. Your consistent, non-judgmental support is a powerful catalyst for their long-term healing and recovery.
This kind of support is more needed than ever. Anxiety disorders are astonishingly common, affecting an estimated 301 million people globally as of 2019. In the United States alone, about 19.1% of adults have experienced an anxiety disorder in the past year. Yet, despite effective treatments being available, many don't get help, often because of stigma or a lack of awareness. You can explore more 2025 statistics on the global impact of anxiety from TherapyRoute.
Building a Foundation for Support
So, where do you start? Your support can make a real, tangible difference, and it begins with small, consistent actions that build trust and create a safe environment. This might mean learning about their specific triggers or asking what helps them most during an intense moment of panic.
For a quick reference, here are some foundational actions you can take right away.
Foundational Ways to Offer Support Immediately
| Action | Why It Helps | Example Phrase |
|---|---|---|
| Just Listen | Creates a safe space for them to be heard without feeling like a problem to be solved. | "I'm here to listen if you want to talk. No pressure." |
| Validate Their Feelings | Shows you believe their experience is real, reducing feelings of isolation and shame. | "That sounds really tough. I'm sorry you're going through that." |
| Offer Reassurance | Reminds them they aren't alone and that the feeling will pass, pointing toward recovery. | "I'm not going anywhere. We can get through this together. You will get better." |
| Ask How You Can Help | Empowers them by letting them guide the support, rather than assuming you know best. | "What would feel most helpful for you right now?" |
Taking these initial steps shows you're in their corner, ready to support them in a way that truly helps.
Here are a few other practical ways to build on that foundation:
- Offer to just listen: Sometimes, the best thing you can do is let them talk through their fears without offering unsolicited advice. Just being a sounding board is powerful.
- Encourage small steps: Instead of pushing them to face huge fears all at once, celebrate the small victories. Each one is a step toward recovery.
- Learn coping tools together: You can explore simple, effective methods to manage acute symptoms. For a great starting point, check out our guide on grounding techniques for anxiety.
By focusing on hope, validation, and practical support, you shift from being a worried bystander to an active, compassionate ally. This approach empowers your loved one, reminding them that they are not alone and that a calmer, more peaceful life is entirely within reach.
Understanding What Anxiety Truly Feels Like

To genuinely help someone with anxiety, you have to look past the dictionary definition. It’s so much more than "worrying" or feeling a little stressed. For the person living it, anxiety is a powerful, full-body experience that can completely hijack their thoughts, feelings, and physical state.
Imagine their mind is a radio stuck between stations, blaring static and alarming news bulletins they can’t turn off. That internal noise isn't just in their head—it shows up in very real, physical ways. It’s the sudden, heart-pounding panic when they’re trying to fall asleep. It's that tightness in their chest that makes taking a full breath feel impossible.
For many, it's a constant, low-level hum of dread, a persistent feeling that something is about to go terribly wrong. Being in that state of high alert is exhausting, making even small, everyday tasks feel like climbing a mountain.
The Lived Experience: What’s Happening on the Inside
Anxiety often operates in stealth mode. While you might see someone who looks perfectly calm, they could be fighting a fierce internal battle. You can’t see the war, but it’s happening.
Here’s a glimpse into what that hidden experience can feel like:
- Catastrophic Thinking: Their brain automatically jumps to the worst-case scenario. A mild headache isn't just a headache; it’s a brain tumor. A friend not texting back immediately means they’re angry or, worse, have been in an accident.
- Looping Thoughts (Rumination): They might replay a past mistake or a simple conversation over and over, analyzing every word and spiraling into self-blame. This isn’t a choice; it feels like a mental hamster wheel they can’t get off.
- Physical Sensations: These can be intense and genuinely frightening, often mimicking serious medical emergencies. We're talking about dizziness, trembling, sweating, shortness of breath, and nausea—all very real sensations.
Getting this is the first real step toward empathy. It’s not about them "overreacting." It's about them reacting to a very convincing internal alarm system that’s gone haywire.
When you support someone with anxiety, you aren't fighting their imaginary monsters. You are sitting with them in the dark until they remember where the light switch is. Your presence reminds them that the feelings are temporary and that they have the strength to get through it and heal.
Demystifying Different Anxiety Disorders
Just like "heart disease" is a broad category, "anxiety" is an umbrella term. Knowing the specific type of anxiety your loved one might be dealing with can help you offer more targeted, effective support.
While only a mental health professional can provide a diagnosis, understanding the common patterns can build your empathy. To get a deeper view, you can explore our detailed guide on https://anxietychecklist.com/anxiety-disorders.
Here are a few common types:
- Generalized Anxiety Disorder (GAD): This is marked by excessive, persistent worry about a wide range of things—health, money, family, work—often without a clear or proportional reason.
- Panic Disorder: This involves sudden, intense episodes of fear called panic attacks. A defining feature is the intense fear of having another attack, which can lead people to avoid places or situations.
- Social Anxiety Disorder: This is an intense fear of being watched, judged, or scrutinized by others. It goes far beyond shyness and can make everyday social interactions feel terrifying.
Recent world events have shown just how vulnerable we all are to these feelings. A 2022 report from the World Health Organization found that the first year of the COVID-19 pandemic triggered a 25% increase in the global prevalence of anxiety and depression. Stressors like social isolation, financial worries, and fear of illness created a perfect storm.
This just goes to show that anxiety is a human response, not a personal failing. With the right support and tools, healing isn't just possible—it's expected.
Effective Communication: What to Say and What to Avoid
When someone you care about is caught in the grip of anxiety, your words can either be a lifeline or an anchor. The right phrase can make them feel seen and understood, but a well-intentioned comment can sometimes feel like a dismissal. Learning how to help often starts with choosing your words carefully.
Your goal isn't to "fix" them or argue them out of their feelings. It's about creating a safe space where their reality is acknowledged. This simple shift can be the difference between them feeling more alone or feeling deeply supported on their path to healing.
The Power of Validation Over Dismissal
One of the most common mistakes is trying to rationalize the anxiety away. Phrases like, "Just relax," or "You're overthinking it," are usually meant to soothe. But to the person struggling, it can sound like you're saying their feelings are wrong or overblown, which only adds shame to the mix.
Validation is the antidote. It doesn’t mean you agree with the anxious thoughts. It just means you accept that their feelings are real for them in that moment.
Your job is not to be the judge of their feelings, but the witness. A simple, "That sounds incredibly difficult," validates their struggle without validating the fear itself. It sends a powerful message: I'm with you, and I believe you have what it takes to get through this.
This small change can open the door to a real conversation. When someone feels understood instead of judged, they’re much more likely to be open to help and begin their journey toward recovery.
The image below shows just how differently people perceive various communication styles when they're looking for support.
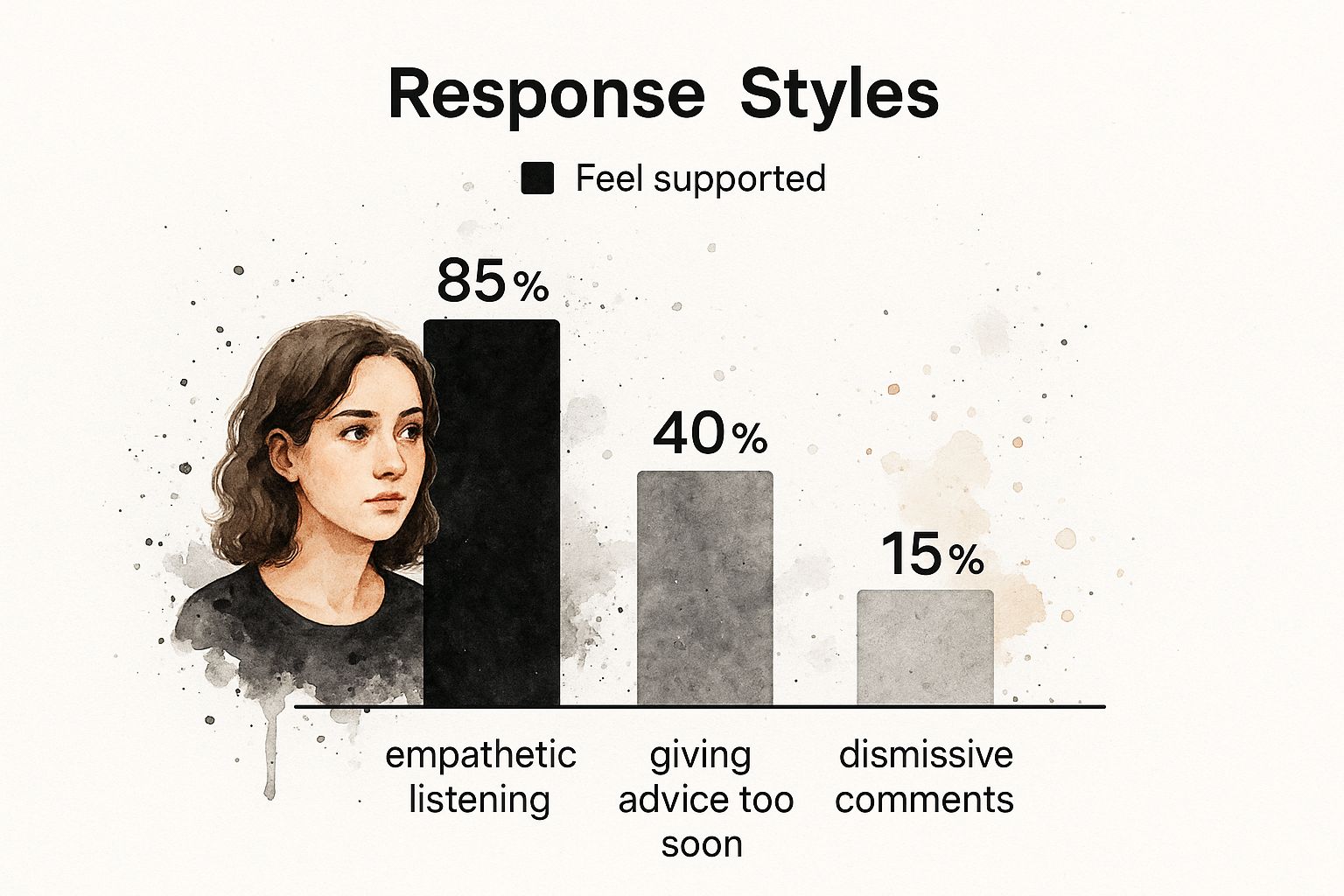
As you can see, empathetic listening is far more effective than jumping in with advice or making comments that feel dismissive. Connection and understanding are truly the most powerful tools you have.
Guiding the Conversation With Helpful Language
So, what does supportive language actually sound like? It’s often simpler and more open-ended than you might think. It’s about asking, not telling. Listening, not lecturing. Your words can gently guide them toward their own strength, reminding them they have the capacity to navigate this and heal.
Knowing what to say—and what not to say—can make all the difference. Here’s a quick guide to swapping common unhelpful phrases for more supportive alternatives.
Helpful vs. Harmful Communication
| Instead Of Saying This… | Try Saying This… | Why It Works Better |
|---|---|---|
| "Don't worry about it." | "I can see this is really weighing on you. What's on your mind?" | This opens a dialogue instead of shutting it down. It shows you're willing to listen to their specific concerns. |
| "You just need to be positive." | "This feels overwhelming right now, but we can get through it. I'm here with you." | It acknowledges the difficulty while offering reassurance and a sense of teamwork. The focus is on getting through it, not just thinking differently. |
| "Have you tried yoga/meditation/etc.?" | "What has helped you feel even a little bit better in the past? Is there anything I can do to help you on your path to feeling better?" | This empowers them by centering their own experience and asking for their lead, rather than imposing a solution they may have already tried. |
| "There's nothing to be afraid of." | "I understand that you feel scared right now. This feeling is temporary, and it will pass." | This validates their emotional state as real, even if the threat isn't. It builds trust and shows you're genuinely trying to understand their reality. |
Choosing your words with empathy turns a monologue into a partnership, reinforcing that you’re on their team.
Fostering Hope and Forward Momentum
Your communication can also be a powerful way to instill hope. Anxiety often paints a picture of a future filled with danger and a present that feels unbearable. Your words can offer a counter-narrative—one of resilience, progress, and the very real possibility of a life that isn't ruled by fear.
Here are a few ways to do that:
- Remind them of their strength. Gently point out times they've successfully handled something tough. "I remember how anxious you were before that presentation, and you did an amazing job. You've handled hard things before and you can do it again."
- Focus on the "now." Anxiety loves to live in the future ("what if…"). Bringing the conversation back to the present moment can be grounding. "Let's not worry about next week just yet. What's one small thing we can do right now to make this moment a little easier?"
- Use "we" language. Phrases like "We can figure this out" or "We'll take it one step at a time" create a sense of partnership. It’s a powerful reminder they aren’t carrying this burden alone.
Every conversation is a chance to reinforce that healing is a journey, not a destination. By communicating with empathy, patience, and hope, you become a vital part of that journey, helping your loved one believe in their own ability to heal and live a life free from panic.
How to Help During a Panic Attack

Watching someone you care about have a panic attack is terrifying. Your own heart might start to race as you see them grapple with what feels like an invisible threat. It's easy to feel powerless, but your calm presence can be the anchor they desperately need to ride out the storm.
During an attack, their body's fight-or-flight system is working overtime, flooding them with adrenaline. Their brain is screaming that they're in mortal danger, even when everything around them is safe. Your job isn't to fix it—it's to be a safe, grounding force until the wave of panic recedes.
And remember, a panic attack always ends. Every single one. Reminding them—and yourself—of this fact is a powerful first step. By staying calm, you offer a sense of safety they can borrow until they find their own again, reminding them that healing is a process and this is just one moment.
Be Their Calm Anchor in the Moment
When a panic attack hits, the person feels completely out of control. Your steady, calm demeanor can be a lifeline in their internal chaos. Speak in a soft, simple, and reassuring voice. Now is not the time for a lot of questions or complex instructions.
Think of yourself as a lighthouse, not a rescue helicopter. You don’t need to swoop in and solve anything. Just be a stable point of light, showing them the way back to shore.
Here are a few things to keep in mind:
- Ask Before Touching: For some, a gentle hand on the arm is grounding. For others, it’s too much. Just ask, "Would it be okay if I put my hand on your shoulder?"
- Give Them Space: Stay nearby, but don't crowd them. Let them have the physical space to breathe or move if they feel the need.
- Use Simple, Reassuring Phrases: Stick to short, supportive statements that cut through the noise.
"You are safe. I'm right here with you. This feeling will pass. You are strong enough to get through this."
This kind of direct, calm communication can break through the mental static of the panic, reassuring them that they're seen, supported, and safe.
Guide Them Back to the Present
Panic attacks often create a sense of detachment from reality, which is incredibly frightening. Grounding techniques are designed to pull their focus away from the scary internal sensations and back to the physical world around them. One of the most effective tools is the 5-4-3-2-1 technique.
You can gently guide them through it:
- "Can you name 5 things you can see right now?" (e.g., a lamp, a blue book, your shoes)
- "What are 4 things you can feel?" (e.g., the chair beneath you, the texture of your jeans)
- "Tell me 3 things you can hear." (e.g., the hum of the refrigerator, a car outside)
- "Can you name 2 things you can smell?" (e.g., coffee, a candle)
- "What is 1 thing you can taste?" (e.g., water, a piece of mint)
This simple process forces their brain to engage with their immediate environment, which helps interrupt the feedback loop of fear. For a deeper look at what's happening in their body and mind during an episode, our guide to the symptoms and stages of a panic attack offers more insight.
After the Attack Passes
Once the peak of the panic subsides, the person will likely feel completely drained, exhausted, and maybe even a little embarrassed. This is a critical time for continued support. Don't just act like nothing happened.
Offer them a glass of water and encourage them to just sit quietly for a few minutes. This isn't the time to dissect the attack or ask what triggered it. Instead, just offer simple comfort.
Reassure them with phrases like, "You did great. You got through it." This reinforces their own strength and resilience. Every time they make it through an attack, it’s a victory. Your support in these moments helps them believe that they have the power to face this and ultimately overcome it.
Encouraging Professional Help and Long-Term Healing
Your support is an incredible gift, but it’s not a substitute for professional care. Encouraging a loved one to seek help is one of the most powerful things you can do, and it is a crucial step on the path to lasting recovery.
The key is to frame it as an act of profound love and strength—not a criticism or a sign that they've failed. Think of it this way: if they had a broken bone, you’d lovingly drive them to a doctor to get it set. Mental health is no different.
It’s about empowering them to take that next brave step toward real, lasting recovery. The ultimate goal isn't just to manage anxiety, but to heal from it and rediscover a life that isn't defined by fear. A life free from panic isn't just a dream—it's an achievable reality.
Framing the Conversation with Compassion
How you approach this conversation matters. Immensely. Avoid ultimatums or making therapy sound like a last resort. Instead, introduce it as a proactive step toward getting better tools and strategies, something that shows courage and self-respect.
Start by expressing your own feelings, using "I" statements to show your concern without placing blame. For instance, you could say, "I've noticed how much you've been struggling lately, and it hurts me to see you in pain. I believe you can get better, and I was wondering if talking to someone who specializes in anxiety might offer some new tools for us to try."
The goal is to open a door, not push them through it. Presenting therapy as a resource for them to become stronger and more resilient can shift their perspective from seeing it as a weakness to seeing it as a tool for empowerment and healing.
Make it crystal clear that you're on their team. You can offer to help with the logistics, which often feel overwhelming to someone already depleted by anxiety. This collaborative approach makes the process feel less isolating and more like a shared mission toward a brighter future.
Practical Ways to Offer Support
Taking that first step can feel monumental. By offering concrete, practical help, you can break down the process into smaller, more manageable actions. This shows your commitment and removes real-world barriers that might be holding them back.
Here are a few specific ways you can help:
- Research Together: Offer to help them find therapists or doctors who specialize in anxiety. You can look at online profiles, read reviews, and check insurance coverage side-by-side.
- Help with Scheduling: Making phone calls can be a major source of anxiety. Simply offering, "Hey, want me to make that first call for you?" or sitting with them while they do it can be a huge relief.
- Go with Them: For that first appointment, offer to drive them or even just wait in the waiting room. Knowing they have an ally right there provides immense comfort.
- Normalize the Experience: Remind them that millions of people see therapists. It’s as normal as going to a physical trainer for fitness or a dentist for your teeth.
Understanding the landscape of anxiety can also help you tailor your support. Severity plays a huge role; in the U.S., while about 19.1% of adults have had an anxiety disorder in the past year, the impact varies. Data shows 43.5% experience mild impairment, 33.7% moderate, and 22.8% serious impairment. This just underscores that there's no one-size-fits-all solution, and finding the right professional is key to their healing journey.
Inspiring Hope for a Panic-Free Future
The most important message you can deliver is one of hope. Anxiety has a way of making the future seem bleak and scary, but effective, evidence-based treatments exist. For a deeper dive into therapeutic options, you can read more about how psychotherapy for anxiety works in our detailed article.
Cognitive Behavioral Therapy (CBT), for example, is highly effective at helping people reframe anxious thought patterns and build new, healthier habits. For some, medication can also be a life-changing tool that calms the nervous system enough for the therapeutic work to really take hold.
Beyond professional support, various self-management tools can be incredibly beneficial. You might encourage them to explore bullet journaling as a self-management tool to help organize thoughts and track moods. By combining professional guidance with personal strategies, they can build a robust toolkit for long-term well-being.
Your belief in their ability to heal is contagious. Remind them that they are not broken and their anxiety does not define them. They are a whole person who is simply struggling with a treatable condition. With the right support system—including you and a qualified professional—a vibrant, panic-free life is absolutely within reach.
Frequently Asked Questions About Anxiety Support

When you're supporting someone with anxiety, you're bound to have questions. This is a journey, and navigating it alongside your loved one will bring up specific challenges and plenty of gray areas.
This section is designed to tackle those common concerns head-on. My goal is to give you clear, practical guidance so you can offer support that’s both compassionate and genuinely helpful.
These answers are here to empower you and reinforce one crucial message: healing is always possible. With the right mix of patience, understanding, and strategy, you can be a powerful force for good in their life.
What If They Refuse to Get Help?
This is easily one of the most common and gut-wrenching situations. You can see the struggle clear as day, but they just aren't ready or willing to seek professional help. Your first instinct might be to push, but I’ve seen that backfire time and again, creating even more resistance.
The most important thing you can do here is to maintain a supportive, non-judgmental presence that is filled with hope.
Keep the lines of communication open. You can say something gentle like, "I'm always here for you when you feel ready to talk or maybe look at some options. I'm not going anywhere, and I believe you can feel better." Your steady support builds a foundation of safety they can rely on.
It also helps to keep educating yourself about anxiety. You can share what you learn in a casual way, without turning it into a lecture. Another powerful approach is to lead by example—talk openly about how you manage your own stress or when you see your doctor for check-ups. This helps normalize the very act of seeking help.
Above all, you have to accept that you can't force someone to change. Your role isn't to be their rescuer; it's to be their anchor of hope. By being a consistent, loving presence, you create an environment where they might eventually feel safe enough to take that brave step—on their own terms.
And don't forget to protect your own well-being. Set healthy boundaries to avoid burning out, and remember that their readiness is not a reflection of your support.
How to Support Without Enabling Avoidance
Ah, the tightrope walk. You want to be compassionate, but you don't want to accidentally reinforce the very avoidance behaviors that keep anxiety in charge. The secret is to validate their feelings while gently encouraging progress toward healing.
Let’s say they're terrified of a social gathering.
- Enabling sounds like this: "Okay, you're right, we just won't go. You don't have to."
- Supporting, on the other hand, sounds like this: "I hear you, and I know you're feeling really anxious about this party. That's completely understandable. How about we try going for just 30 minutes together? I'll stay right by your side, and we can leave the second you want to."
This approach does a few crucial things:
- It acknowledges their feelings as real and valid.
- It offers a collaborative, step-by-step solution instead of total retreat.
- It positions you as their safety net, which can give them the courage to try.
The goal is to encourage small, manageable steps outside their comfort zone. If their anxiety is tied to social situations, getting a deeper understanding can be a game-changer. You can learn more by reading about the challenges and strategies related to Social Anxiety Disorder in our detailed guide.
No matter the outcome, always praise their courage for trying. This builds resilience and shows them that their effort—not just the "success"—is what truly matters on the path to living panic-free.
How Can I Avoid Caregiver Burnout?
Supporting someone with anxiety is emotionally draining, and caregiver burnout is a very real risk. If you run on empty, you can't offer effective support. Prioritizing your own mental health isn't selfish; it's absolutely essential for both of you to sustain the journey toward healing.
First, establish clear and healthy boundaries. It is 100% okay to say, "I need an hour to myself to recharge, but I'd love to connect with you after that." This protects your energy while still showing you care.
Second, maintain your own life and routines. Don't let their anxiety swallow your world whole. Keep up with your own hobbies, friends, and interests. These are the things that will refill your cup and keep you grounded.
Third, build your own support system. You need someone to talk to, too. Whether it's a trusted friend, a family member, or your own therapist, having an outlet to share your frustrations and feelings is non-negotiable. You can't be the only support system without having one yourself.
Finally, practice self-compassion. You won't always say or do the perfect thing, and that's okay. You're doing your best in a tough situation. Remember, by taking care of yourself, you model healthy behavior and ensure you can remain a strong, hopeful presence for the long haul.